A new study from the California Workers' Compensation Institute (CWCI) found drug tests have been added to more Workers' Compensation pain management programs in published treatment guidelines throughout the state of California. The increased use of opioids over the past decade and growing concerns about the long-term reprecussions have influenced this increase, says CWCI.
In the report, titled "The Utilization and Cost of Drug Testing in the California Workers' Compensation System," CWCI analyzed a database of 2.8 million clinical lab service records for urine drug tests (UDTs) performed on California injured workers between 2002 and 2014, for which claims administrators paid $108 million. According to Stacy Jones, CWCI senior research associate, UDTs as a percentage of all California WC lab services increased nearly six-fold over the last eight years — 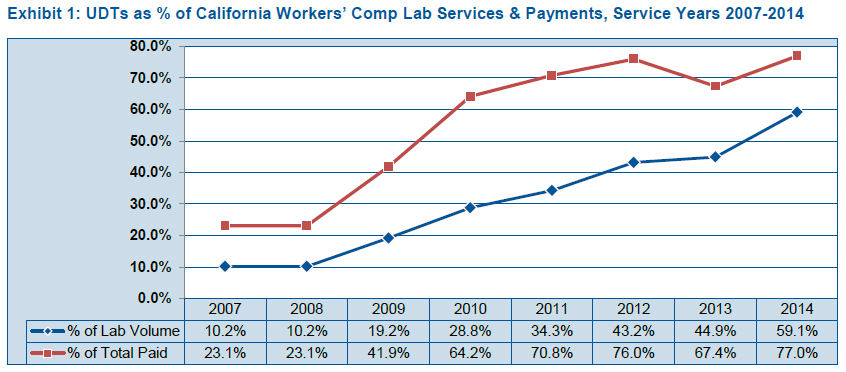 from 10.2% in 2007 to 59.1% in 2014. As a result, UDT payments went up from 23% to 77% of WC lab payments over the same period.
from 10.2% in 2007 to 59.1% in 2014. As a result, UDT payments went up from 23% to 77% of WC lab payments over the same period.
(Click the chart on the right for full size.)
Recommended For You
Want to continue reading?
Become a Free PropertyCasualty360 Digital Reader
Your access to unlimited PropertyCasualty360 content isn’t changing.
Once you are an ALM digital member, you’ll receive:
- Breaking insurance news and analysis, on-site and via our newsletters and custom alerts
- Weekly Insurance Speak podcast featuring exclusive interviews with industry leaders
- Educational webcasts, white papers, and ebooks from industry thought leaders
- Critical converage of the employee benefits and financial advisory markets on our other ALM sites, BenefitsPRO and ThinkAdvisor
Already have an account? Sign In Now
© Touchpoint Markets, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more inforrmation visit Asset & Logo Licensing.







